ResultsCX Case Study
Global customer experience (CX) management leader, ResultsCX, averages 10 years’ tenure among top 10 clients and 93% customer retention. As a part of the company’s mission to power CX growth, ResultsCX tapped conversation intelligence platform CallMiner to dig into the “why” behind clients’ contact drivers and develop a comprehensive strategy to drive customer satisfaction and retention. By analyzing 100% of customer interactions, the team delivered strategic analysis to a healthcare client to prevent customer churn, improve satisfaction, and drive successful sales outcomes.
Challenges
Health insurance provider struggled to understand customer complaints and adherence to scripting
The ResultsCX team is constantly looking for ways to drive CX improvements for its clients. One major health insurance provider wanted to understand customer complaints and adherence to scripting, and develop an improvement plan for how agents handled both retention and sales opportunities.
Prior to adopting conversation intelligence, reports were transactional and focused on baseline quality outcomes. The ResultsCX team wanted to dig beyond their current reporting capabilities to understand the true root cause behind customer contact drivers. To do that, they required a more robust analytics system than the one they were using for basic quality scorecards.
“We needed a solution to help our clients with specific use cases, such as digging into the ‘why’ behind lost revenue,” said Aaron Prisco, VP of Client Solutions, ResultsCX. “We want to improve agent performance based on behavior – and provide more strategic analysis for our clients’ CX decision-makers.”
Specifically, to understand their health insurance clients’ customer complaints and agents’ sales strategies, they needed to drill into specific language and terminology agents were using during customer interactions. ResultsCX helped the client focus on three key challenge areas – from there, they could develop a strategic action plan that would improve contact center performance and drive more revenue.
- Differentiating customer grievances – Most of the client’s customer calls fell into two buckets – customers that were navigating a scenario where their plan was going away and customers who are 65 and over who are calling in for general claims. The client needed help in identifying and differentiating those different call drivers.
- Increasing sales-compliant language – In the scenarios where customers were calling in because they needed to choose a new plan, the client wanted to see certain sales compliance language being used. This included agents properly guiding the conversation in terms of upselling customers to a new plan so they wouldn’t go to another provider.
- Mandatory compliance and script adherence – Insurance is a regulated industry, which means there are mandatory compliance statements when making certain calls. To do this properly, agents can’t just check boxes. Getting script adherence right means stopping at the right moments and confirming customer understanding, in addition to hitting verbal compliance statements.
In relation to sales-compliant language, Scott Stacy, Senior Director, Insights and Analytics, ResultsCX, said: “Today, the team can see that sales-compliant language is being used in 70% of calls. We have a target benchmark of 90% and are planning to implement coaching strategies on how agents can make more effective use of sales language to close more deals. One thing we’re considering is tracking agents that have successfully closed the most deals and pulling best practices and strategies from these agents to implement with the rest of the team.”
Solution
Gaining contextual insight into customer feedback with CallMiner Enhanced AI Module
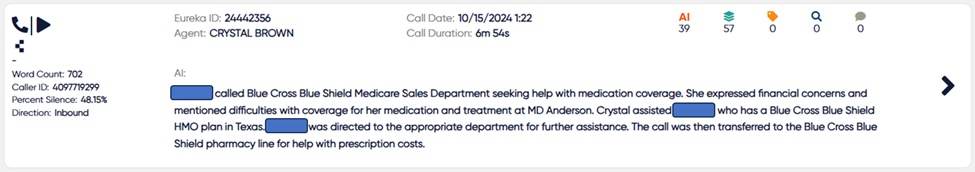
The ResultsCX team selected CallMiner to analyze 100% of customer interactions, construct queries, and uncover key business insights from these interactions. As part of CallMiner’s Enhanced AI Module, the team used AI classifiers that leverage LLMs to automatically label the context of those interactions. With CallMiner’s generative AI, ResultsCX can now automatically evaluate customer conversations based on similar interactions, reducing the time and effort they need to gain critical insights to drive business decisions.
In addition, the ResultsCX team uses CallMiner’s semantic search to automatically discover insights within clients’ omnichannel customer interactions. Using natural language statements, they can view results with similar meanings, rather than building out search categories with syntax. Searching for contextual meaning returns faster business insights around contact center efficiency, CX improvement, and more.
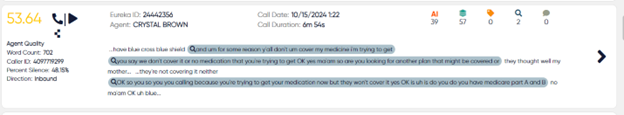
For their health insurance client, ResultsCX searched for specific trigger language and terminology around retention and sales. This language ensures agents are using the correct words and phrases to avoid customer churn, as well as improve satisfaction and drive sales outcomes. Over the course of 90 days, the team ingested 42,000 customer interactions into CallMiner, using generative AI tools to provide insights to their healthcare clients’ decision-makers.
“CallMiner’s AI revealed key insights about the symptoms, root causes, and ramifications behind customer complaints,” said Brock Duffel, Director of Insights and Analytics, ResultsCX. “The results showed that not all sentiment was negative or a ‘complaint,’ so we took a higher-level contextual view based on actual conversations.”
Results
Delivering strategic analytics to clients, while improving agent performance
Digging a layer deeper, ResultsCX found that less than 50% of the health insurance client’s customer complaints were actual complaints about the company. Instead, approximately 85% of calls were driven by coverage complaints. For example, customers contacted the company with confusion about their coverage and benefits, or concerns and feedback about their doctors, medications, and services provided.
They were able to break down complaints further into cost/affordability and hardship issues including copays/deductibles, services, and bills. By understanding which customers called about affordability vs. confusion and understandability, they were able to pinpoint the cause of customer dissatisfaction – recommending specific coaching improvements and retention skills. Even though 70% of calls were hits for “escalations,” many of these calls were resolved positively and effectively.
The ResultsCX team is now working with the health insurance company to increase efforts on communication and awareness of benefits and coverage during enrollment. The recommended course of action is to provide introductory and refresher training for agents on escalation calls and sales language to improve performance.
“CallMiner enables us to ‘drill down’ and pinpoint specific topics or subjects within calls, especially with its expanded capabilities [AI tools]; it truly can be a performance-enhancer with projects such as this,” said Diana Geisler, Director of Account Operations, ResultsCX.
In the future, the team has plans to analyze even more data in CallMiner, and develop data-driven plans to meet and exceed the health insurance company’s customer retention goals. AI will play a major role in doing this efficiently and strategically in this and future client engagements.

